WHF-SCORECARD-2022-GHANA(Dev3)
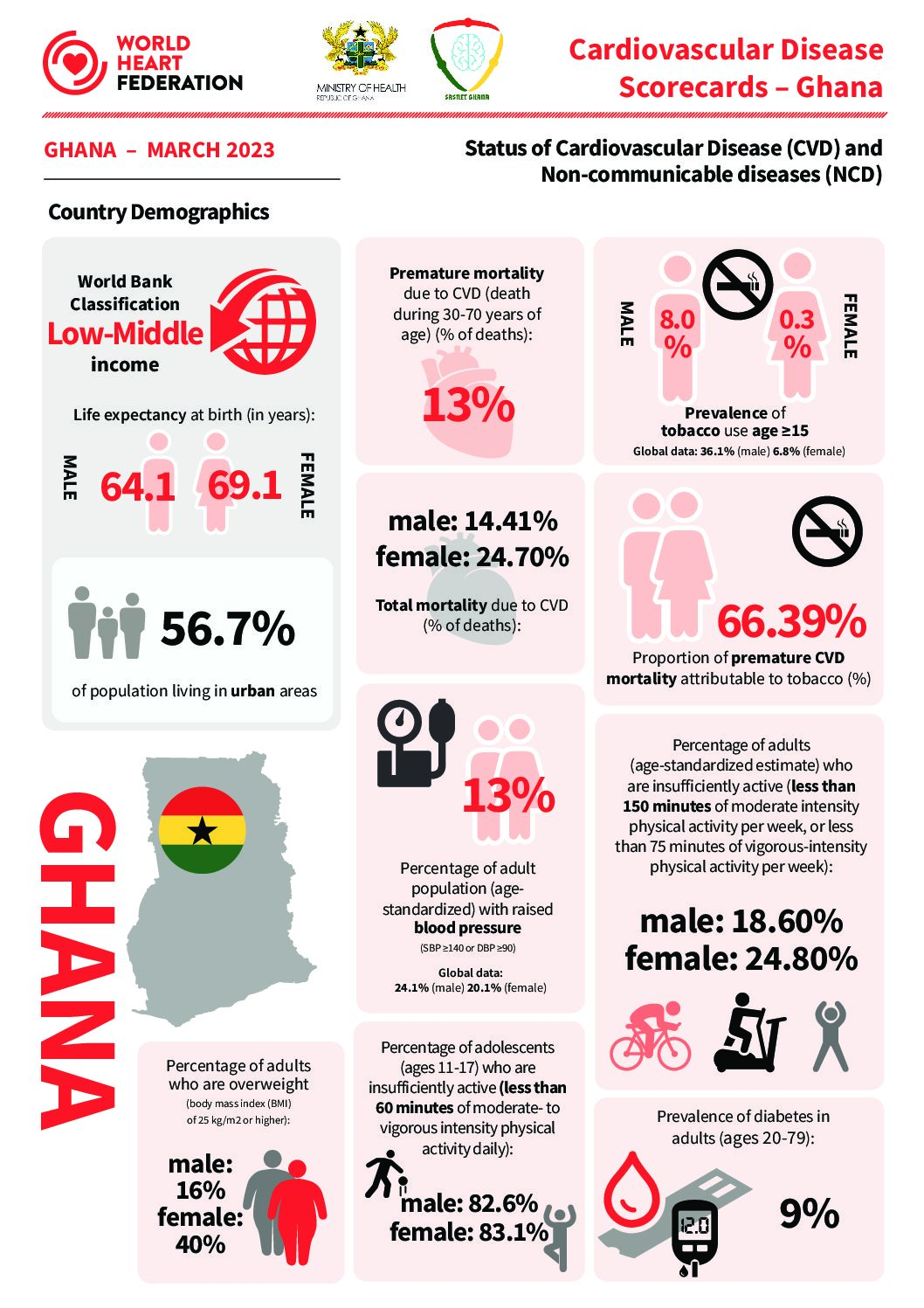
Summary of Ghana’s CVD Scorecard
The world over, Non-Communicable diseases (NCDs) have become a major public health concern with attendant negative implications on the lives and development of the individuals, the family, community, the nation and beyond. NCDs undermine the attainment of development targets at various levels through social, economic, and biological pathways in a vicious cycle of ill-health, poverty, strained family cohesion, poor mental health, productivity loss among others. The burden of mortality attributed to these NCDs, such as cancer, hypertension, cardiovascular disease, diabetes, stroke, etc. were expected to exceed that of communicable diseases by 2030. However, it is fast becoming obvious that NCDs may be contributing more to indices of morbidity and mortality than communicable diseases.
There is an established double disease burden of Communicable and Non-Communicable Diseases in Ghana, with Non-Communicable Diseases fast gaining prominence as the leading causes of hospital attendance and deaths. NCDs include diabetes, obesity, stroke, hypertension, cancer and others. Some of the afore-mentioned diseases (Hypertension, Diabetes, Obesity, etc.) are known predisposing risk factors for cardiovascular diseases. Indeed, an analysis of the trend of morbidity and mortality for Ghana has shown a rise in the prevalence of CVD related conditions. It is also known that the socio-demographics characteristics of those with CVD and related diseases are rapidly shifting from older age groups to younger ones and currently, individuals at high risk of CVDs are usually at the peak of their productive years.
The objectives of the Ghana NCD Policy include reducing the incidence of chronic NCDs; reducing the unhealthy lifestyles that contribute to NCDs; reducing morbidity associated with NCDs and improving the overall quality of life in persons with NCDs.
As part of efforts aimed at achieving objective of the country’s National Health Policy and NCD Policy is the establishment of systems for the prevention, early detection, prompt management and accurate reporting of CVDs at all Operational Levels.
The results of the CVD Scorecard Project have revealed unsettling trends in the economic burden of CVDs. For instance, the Estimated direct (e.g. health care-related) cost of tobacco use in Ghana’s population stood at 123 million USD every year, i.e. an average per capita of over Fifty – Two Thousand (52,000) persons (i.e. USD 2,363.3). The Proportion of premature CVD mortality attributable to tobacco (%) is estimated at 66.39%. Given the seemingly “low” prevalence of tobacco use, a proposed hypothesis for this could be explained by secondary smoking and the use of other forms of tobacco.
Recorded alcohol consumption per capita (15+ years) in liters of pure alcohol in a three-year period in Ghana averagely stood at 2.7 liters, meaning the entire Ghanaian population consumes 27,713,347.2 liters every year.
A quick look at the afore mentioned figures indicate that Ghana stands to make tremendous health and economic gains from combating CVDs and NCDs in general. The Project has also highlighted the strengths of the Ghanaian health system, such as a strong health workforce base and the availability of the appropriate clinical protocols and guidelines for health care delivery. Bolstering the weak structures of Ghana’s health care system, will afford tremendous gains in reducing morbidity and mortality due to CVDs and improving the quality of lives of Ghanaians.
Contact Ministry of Health Ghana and the project coordinator Ad Adams Ebenezer for the full report via email ad.adams@sasnetghana.org or strokeghana@yahoo.com
SASNET GHANA Secretariat +233(0)594989495
Find Ghana’s CVD Score Card infographic link below