(CNN)The new coronavirus appears to be causing sudden strokes in adults in their 30s and 40s who are not otherwise terribly ill, doctors reported
They said patients may be unwilling to call 911 or (other emergency line) because they have heard hospitals are overwhelmed by coronavirus cases.
There’s growing evidence that Covid-19 infection can cause the blood to clot in unusual ways, and stroke would be an expected consequence of that.
Dr. Thomas Oxley, a neurosurgeon at Mount Sinai Health System in New York, and colleagues gave details of five people they treated. All were under the age of 50, and all had either mild symptoms of Covid-19 infection or no symptoms at all.
“The virus seems to be causing increased clotting in the large arteries, leading to severe stroke,” Oxley told CNN
How can I protect myself from exposure to the new novel corona virus?
Observing personal hygiene and adhering to protocol or directives including physical distancing , frequent and thorough handwashing and wearing of facemask
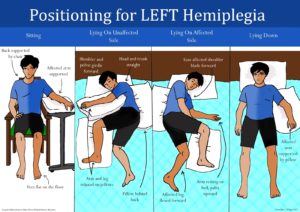
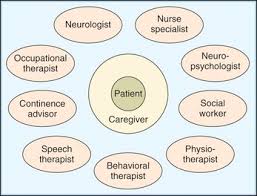
If you have heart or CVD or have had a stroke, these are factors to consider during physical distancing:
Make sure you have a list of contacts – caregivers, healthcare providers, as family members and friends who could help you.
Ensure you have a three months supply of prescriptions (drugs) .
In stocking up on non-perishable foods, give priority to healthy choices(diet with more fruits and vegetables)
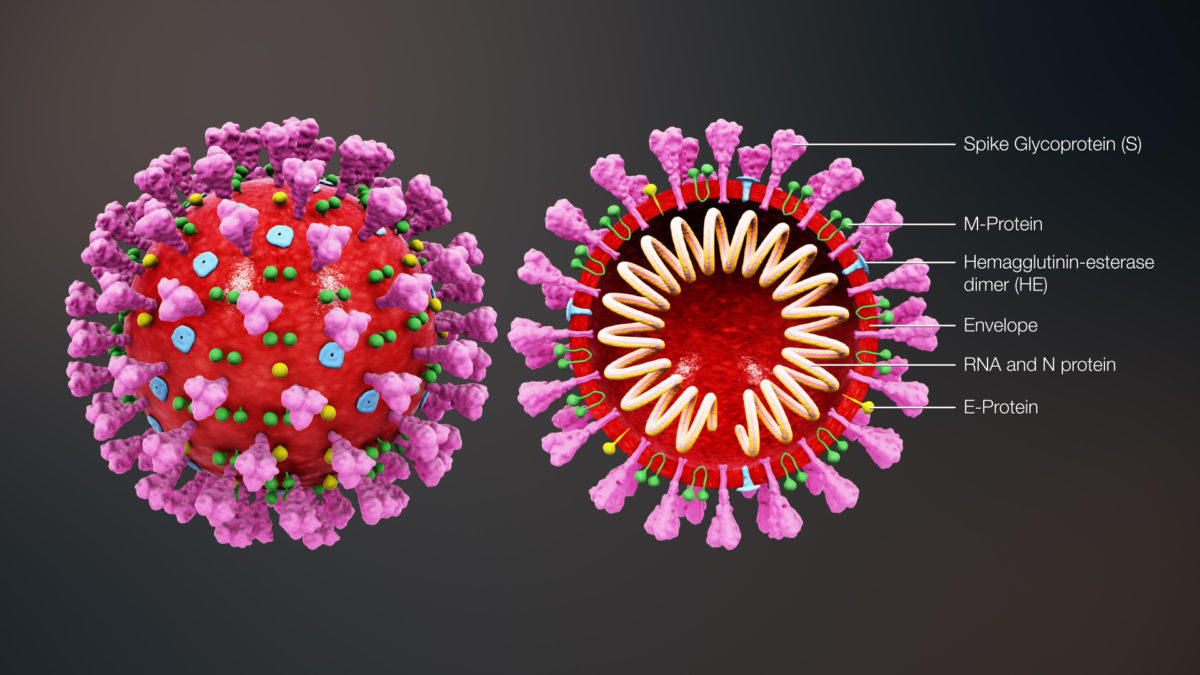
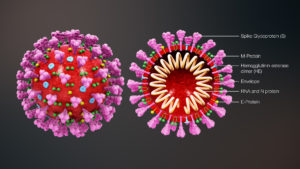
COVID19
Coronavirus disease is an infectious disease caused by severe acute respiratory syndrome coronavirus 2. It was first identified in December 2019 in Wuhan, Hubei, China, and has resulted in an ongoing pandemic.
SYMPTOMS OF COVID19
People with COVID-19 have had a wide range of symptoms reported – ranging from mild symptoms to severe illness. Symptoms may appear 2-14 days after exposure to the virus. People with these symptoms may have COVID-19:
Fever or chills
Cough
Shortness of breath or difficulty breathing
Fatigue
Muscle or body aches
Headache
New loss of taste or smell
Sore throat
Congestion or runny nose
Nausea or vomiting
Diarrhea

What can you do to prevent a Stroke or a Second Stroke?
You can’t reverse the years or change your family history, but there are many other stroke risk factors that you can control(modifiable) —provided that you’re aware of them. **Knowledge is power**. If you know that a particular risk factor is sabotaging your health and predisposing you to a higher risk of stroke, you can take steps to alleviate the effects of that risk.
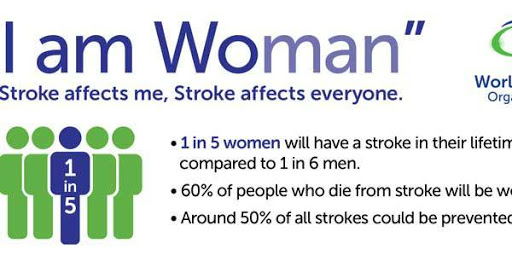
Globally, stroke is a leading cause of mortality and disability and there are substantial economic costs for post-stroke care(Global Burden of Disease ,GBD)
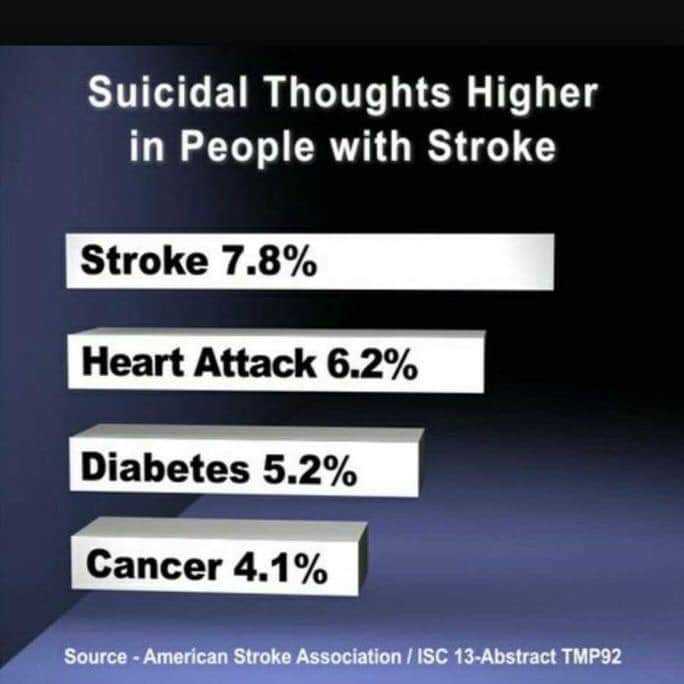
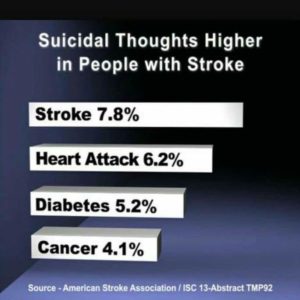
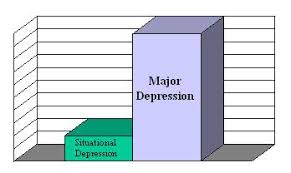
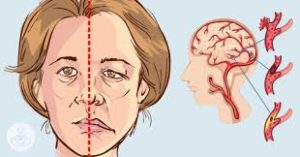
Stroke, the sudden death of some brain cells due to lack of oxygen when the blood flow to the brain is lost by blockage or rupture of an artery to the brain, is also a leading cause of dementia and depression. Globally, 70% of strokes and 87% of both stroke-related deaths and disability-adjusted life years occur in low- and middle-income countries.(Walter Johnson, et al.)
7 ways to Prevent a Stroke or a Second Stroke
Here are seven ways to start reining in your risks today to avoid stroke, before a stroke has the chance to strike.
1. Lower blood pressure
High blood pressure is a huge factor, doubling or even quadrupling your stroke risk if it is not controlled. High blood pressure is the biggest contributor to the risk of stroke in both men and women. Monitoring blood pressure and, if it is elevated, treating it, is probably the biggest difference people can make to their vascular health.
Your ideal goal: Maintain a blood pressure of less than 120/80(with respect to your age) if possible. For some older people, this might not be possible because of medication side effects or dizziness with standing.
How to achieve it:
Reduce the salt in your diet, ideally to no more than 1,500 milligrams a day (about a half teaspoon).
Increase polyunsaturated and monounsaturated fats in your diet, while avoiding foods high in saturated fats.
Eat 4 to 5 cups of fruits and vegetables every day, one serving of fish two to three times a week, and several daily servings of whole grains and low-fat dairy.
Get more exercise — at least 30 minutes of activity a day, and more, if possible. Quit smoking, if you smoke.
Contact your Doctor on your blood pressure medicines and report any side effects when taking these drugs.
2. Lose weight
Obesity, as well as the complications linked to it (including high blood pressure and diabetes), raises your odds of having a stroke. If you’re overweight, losing as little as 10 pounds can have a real impact on your stroke risk.
Your goal: While an ideal body mass index(BMI) is 25 or less, that may not be realistic for you. Work with your doctor to create a personal weight loss strategy.
How to achieve it:
Try to eat no more than 1,500 to 2,000 calories a day (depending on your activity level and your current BMI).
Increase the amount of exercise you do with activities like walking, golfing, or playing tennis, and by making activity part of every single day.
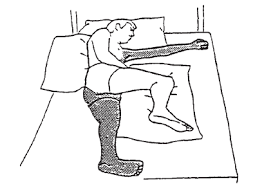
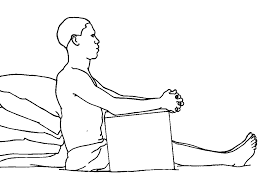
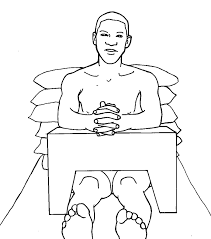
3. Exercise more
Exercise contributes to losing weight and lowering blood pressure, but it also stands on its own as an independent stroke reducer.
Your goal: Exercise at a moderate intensity at least five days a week.
How to achieve it:
Take a walk around your neighborhood every morning after breakfast. Start a fitness club with friends.
When you exercise, reach the level at which you’re breathing hard, but you can still talk. Take the stairs instead of an elevator when you can.
If you don’t have 30 consecutive minutes to exercise, , break it up into 10- to 15-minute sessions a few times each day.
4. If you drink Stop
Drinking alcohol as a person living with Stroke or NCDs is not SAFE to your health. Substitute alcohol with sugar free fruit drink and water . Its not advisable to take alcohol as a person living with Stroke /NCDs .
Your goal: Don’t drink alcohol .
How to achieve it:
Take a lot of water every day and substitute alcohol for sugar free fruit drink .
Seek support from a doctor , a psychologist or support group.
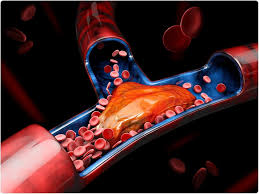
5. Treat atrial fibrillation
Atrial fibrillation is a form of irregular heartbeat that causes clots to form in the heart. Those clots can then travel to the brain, producing a stroke. Atrial fibrillation carries almost a fivefold risk of stroke.
Your goal: If you have atrial fibrillation, get it treated.
How to achieve it:
If you have symptoms such as heart palpitations or shortness of breath, see your doctor for an exam.
You may need to take an anticoagulant drug (blood thinner) such as warfarin (Coumadin) or one of the newer direct-acting anticoagulant drugs to reduce your stroke risk from atrial fibrillation. Your doctors can guide you through this treatment.
6. Treat diabetes
Having high blood sugar damages blood vessels over time, making clots more likely to form inside them.
Your goal: Keep your blood sugar under control.
How to achieve it:
Monitor your blood sugar as directed by your doctor.
Use diet, exercise, and medicines to keep your blood sugar within the recommended range.
7. Quit smoking
Smoking accelerates clot formation in a couple of different ways. It thickens your blood, and it increases the amount of plaque buildup in the arteries. Along with a healthy diet and regular exercise, smoking cessation is one of the most powerful lifestyle changes that will help you reduce your stroke risk significantly.
Your goal: Quit smoking.
How to achieve it:
Ask your doctor for advice on the most appropriate way for you to quit.
Use quit-smoking aids, such as nicotine pills or patches, counseling, or medicine.
Don’t give up. Most smokers need several tries to quit. See each attempt as bringing you one step closer to successfully beating the habit.
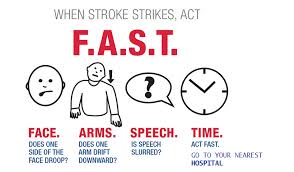
Identify a stroke using the F-A-S-T test
Too many people ignore the signs of stroke because they question whether their symptoms are real. “My recommendation is, don’t wait if you have any unusual symptoms,” Dr. Rost advises. Listen to your body and trust your instincts. If something is off, get professional help right away.”
Signs of a stroke include:
weakness on one side of the body.
numbness of the face.
unusual and severe headache.
vision loss.
numbness and tingling.
unsteady walk.
Harvard Health Publishing (June 2013). 7 things you can to to prevent stroke.

GET FREE SUPPORT : Person living with stroke and their carers can have answers to their mind boggling questions and access information on stroke care and support by signing up to the Post Discharge Stroke Support(PDSS) Program by the Stroke Association Supportnetwork-Ghana (SASNET-GHANA).
Visit our website below for more information
http://:care.sasnetghana.org or email us : info@sasnetghana.org
Helpline + 233594989496 or WhatsApp us +233262463986
Sign up to Ask Dr Charway –Felli Platform for more support from the Professionals
Register for free support online here : care.sasnetghana.org/ask-charway/
NATIONAL STROKE HELPLINE (GHANA) LAUNCHED
CALL 0594989495
Email: helpline@sasnetghana.org